Medical service fees are defined as the fees received by a medical facility or pharmacy in exchange for insured medical services or products provided to an insured person. These fees are overseen by the Ministry of Health, Labour, and Welfare (MHLW), which sets the fee schedule and determines the billing conditions for medical services, medical devices, and pharmaceuticals all providers must adhere to. There are prohibitions against setting fees higher than those in the fee schedule and providers are restricted from combining non-listed services and products with listed ones, with very few exceptions. Mixed medical care series (MMS or kongo shinryo) is currently being introduced and further exceptions to these restrictions are expected in 2016.
Payment System
Fee for Service
Since the system was established in its current form in 1961, healthcare fees have been administered on a fee-for-service (FFS) basis. When a service, pharmaceutical product or medical device is provided through the insurance system, the provider calculates reimbursements based on the number of points allocated for each item. The provider is then reimbursed for the service or product based upon the number of points.
Diagnosis Procedure Combination
Diagnosis procedure combination (DPC) is a uniquely Japanese payment system that first emerged in the early 2000s amidst growing concerns over healthcare costs, length of hospital stays, and the healthcare needs associated with the growing aging population. The goal of DPC is to support improvement in health care standards and transparency. Through the collection of objective treatment information made accessible through a database, this system strives to not only help hospital administrators and providers better understand the outcomes related to the care they are delivering, but also to improve quality of care and address disparities between hospitals. Patients also have access to data-based care standards as well as pricing information. DPC was also designed to shorten the average hospital stay length. As of 2012, this payment system was estimated to cover nearly 53% of general hospital beds in Japan.1
Similar to the diagnosis related groups (DRG) prospective payment system (PPS) found in the U.S., DPC is prospective and uses codes based on diagnosis categories and diagnosis groups. As of April 2012, there were 2,927 DPC codes. The unique part of this payment system, however, is that it is per-diem and integrates standard FFS payments. Providers are paid a flat-rate prospective fee per day of inpatient hospital stay for certain DPC services and paid FFS for non-DPC services.
More specifically, DPC payments:
- Are dispersed for hospital stays, diagnostics, injections, pharmaceuticals, and medical treatments valued at less than 1,000 points. Payments are calculated on a per-day basis depending on the DPC code and medical institution’s coefficient, which was previously unique to each institution. This coefficient is currently being revised to reflect hospital type giving hospitals of similar type across Japan the same coefficient.2
- Do not cover surgery, radiation therapy, anesthesia, and medical treatments valued at more than 1,000 points. These instead are paid FFS.
- Differ according to hospitalization stage. Per-day payments for the first stage are higher than the latter two stages. The second stage lasts until the average length of stay and per-day payments within this stage are set lower effectively neutralizing the higher payment provided in the first stage. Per-day payments for hospitalization within the third and last stage are lower than the payment rates of the second stage. If length of stay becomes exceptionally extended, all payments become FFS.
Various analyses have been conducted to determine whether DPC is succeeding in achieving its intended purposes. While it has largely been shown that DPC has not resulted in lower costs due to its unique mix of PPS with FFS, there is strong opposition against further integration of PPS.3,4,5
What is the specified period of hospital stay?
The specified period of hospital stay divides a hospital stay into three periods. Period 1 refers to the length of time equal to the 25th percentile of the average length of stay (ALS) for the specific episode. Period 2 extends from the 25th percentile to the ALS. Period 3 begins after the patient remains in the hospital after the ALS and lasts until a period equal to the ALS plus 2 standard deviations. Under the DPC system, after a patient exits period 3 and leaves the specified period of hospital stay, medical expenses are reimbursed fee-for-service. See figure below.
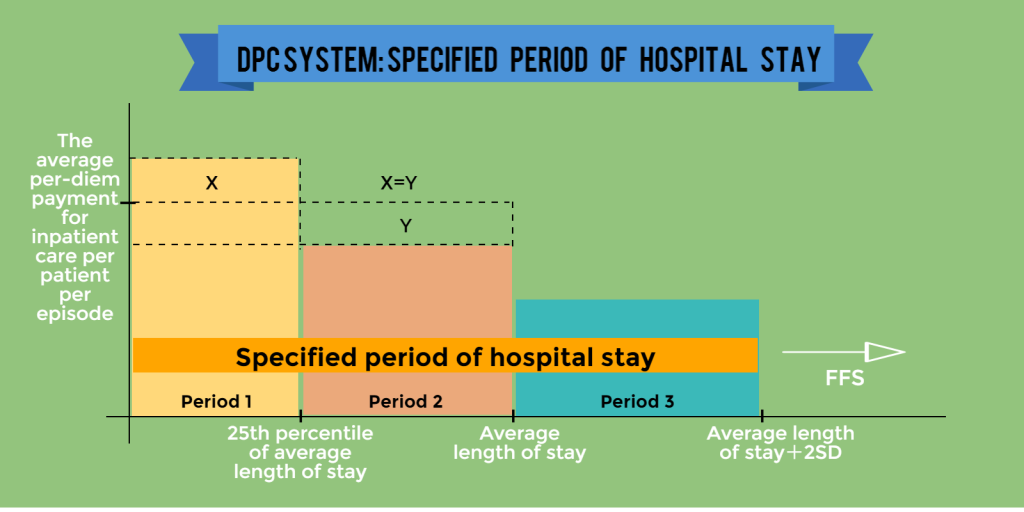
Source: Kinki Regional Bureau of Health and Welfare, 2010 Payment System Revision Overview
Has episode-based payment resulted in lower costs?
Another goal of the Japanese system of episode-based payment was to drive down costs, but is that goal being achieved? Actually, there is a possibility that health care costs have increased as a result of DPC. While DPC was successful in reducing the average length of hospital stay, an increase in the per-diem rate of inpatient care created an incentive for hospitals to increase the number of inpatients. The introduction of DPC also saw the start of “DPC consulting” services that, in some cases, help facilities manipulate coding, or up-code, in order to yield greater returns per patient.
References
1 Ishii, M.( 2012). DRG/PPS and DPC/PDPS as Prospective Payment Systems. The Japan Medical Association Journal. 55(4): 279–291, Retrieved from https://www.med.or.jp/english/journal/pdf/2012_04/279_291.pdf (accessed on 14-07-2015)
2 Ikegami N. Universal Health Coverage for Inclusive and Sustainable Development. Washington, D.C.: World Bank Group, 2014.
3 Yasunaga,H., Ide, H., Imamura, T., Ohe, K. Impact of the Japanese Diagnosis Procedure Combination-based Payment System on Cardiovascular Medicine-related Costs. International Heart Journal. 2005 Sep; 46(5):855-66.
4 Ishii, M. DRG/PPS and DPC/PDPS as Prospective Payment Systems. Japan Medical Association Journal 55 (4): 279-291, 2012.
5 Kondo, A. and Kawabuchi, K. Evaluation of the introduction of a diagnosis procedure combination system for patient outcome and hospitalisation charges for patients with hip fracture or lung cancer in Japan. Health Policy. 2012 Oct;107(2-3):184-93.

